The information provided in this blog is for educational and informational purposes only and is not intended as medical advice. If you have questions about your health, speak to your GP or specialist.
As the year winds down, it is important not to overlook November and the global initiative known as Movember, which provides a dedicated time and space to raise awareness of men’s health – not just heart disease, high blood pressure or prostate or testicular cancer but also mental health.
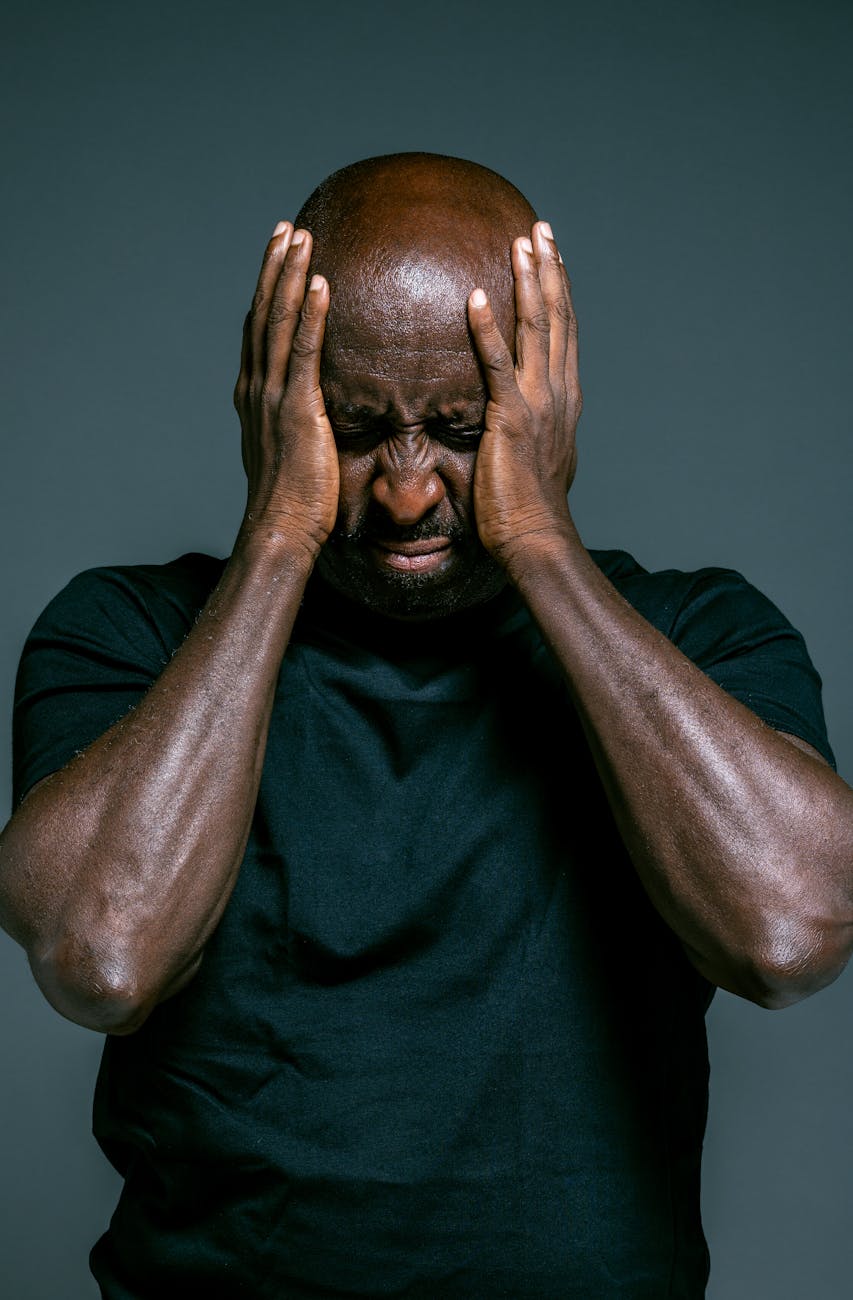
Yet within the broad canvas of men’s mental health, there is a group whose lived experience is marred by persistent inequalities: Black men in the UK. In this week’s blog we explore the social and structural forces that shape Black men’s mental health, and how Movember can contribute meaningfully in this space
What the evidence tell us about access, diagnosis, and outcomes
According to the last Census for England and Wales (source), Black people (including Black African, Black Caribbean, and Black Other) made up 4% of the total population, which equates to around 2.4 million people and of this group, men and boys represent roughly 49%.
The evidence paints a stark picture for Black people’s mental health in England. According to the health regulator, Care Quality Commission (CQC), Black or Black British men are 3 times more likely to be detained under the Mental Health Act than people in white ethnic groups (source).” They are also more likely to be placed on community treatment orders (CTOs) and to have longer hospital stays (source). Black men (of African and Caribbean heritage) are 5 times more likely than white men to receive a diagnosis of schizophrenia and to be admitted to hospital, yet are less likely to access care early (source).
One study of help seeking behaviour among Black family members in the UK and Nigeria found that cultural and structural barriers (including stigma, the idea “a man should be strong”, and poor knowledge of services) inhibited seeking professional help (source). Another study specifically on Black men’s experience of psychosis found that oppressive experiences such as racism, powerlessness, marginalisation were central to how Black men interpreted their encounters with mental‑health services (source).
In short: Black men are over‑represented in the most restrictive parts of the mental health care provision (detention, involuntary treatment) while being under‑represented in early supportive interventions. Their pathways into care often reflect crisis rather than prevention.
Why are these inequalities happening?
Structural racism and discrimination in services: mental‑health services in England are often not designed to provide culturally competent care and address or even recognise how institutional racism affects Black men’s access and experience of care (source). The CQC, healthcare regulator for England has concluded that services need to be “anti‑racist, co‑produced and community‑based” to be effective for Black men.
Masculinity social norms and help‑seeking barriers: dominant social norms of masculinity such as the belief that men should “be strong” ,“be a man”, “don’t let them see you sweat” and “handle it” often discourage vulnerability and help-seeking. For Black men, these pressures are compounded by racialised expectations and a deep-rooted distrust of services.
A mixed methods study cited “the perception that a man should be strong” as a key barrier to accessing support (source). While quantitative data specific to Black men in the UK remains limited, qualitative findings confirm recurring narratives of marginalisation, with many entering care through crisis rather than choice (source).
Research from the Race Equality Foundation (source) and other organisations shows that stigma, fear of being misunderstood, and previous negative experiences with services are common barriers that prevent Black men from accessing timely mental health care.
Socio‑economic disadvantage and life burdens: for younger Black men, the pandemic impact (job‑loss, disrupted education, increased policing/stop‑and‑search) had real mental‑health consequences. (source) Discrimination more broadly (“weathering”) has known links to poorer mental‑health outcomes. A higher prevalence of common mental disorders in Black/Black British adults (23% vs white British 17%) in a mental‑health snapshot. (source).
Emergent contributory factors: other contributors that are less researched include intergenerational trauma and toxic masculinity, as key contributors to the mental health crisis among Black men. These burdens are compounded by economic hardship and limited access to culturally sensitive support (source).
Pathways into care via crisis rather than prevention: because Black men are less likely to access early care, they are more likely to reach services via acute or criminal justice routes. Research on Black men’s psychosis experiences identified that many entered care through police or custody rather than voluntarily (source).
The information provided in this blog is for educational and informational purposes only and is not intended as medical advice. If you have questions about your health, speak to your GP or specialist.
Recognising Mental Health Struggles: Tools for Black Men and Their Communities
While Black men in the UK are disproportionately represented in crisis care such as being detained under the Mental Health Act, many others experience ongoing mental health challenges that don’t reach crisis point but still significantly affect their wellbeing. Studies and community reports highlight that many Black men may not have access to culturally competent mental health education or services. This can lead to difficulty recognising symptoms of mental distress or knowing where to turn for support. Also, fear of being misunderstood or judged by predominantly white services leads to avoidance of care.

Signs and symptoms
Black men, like many others, don’t always show mental health struggles in the ways we expect. Instead of sadness or tears, it might come out as anger, irritability, emotional shutdown, or risky behaviour. Social pressures to “man up” or stay quiet about emotions often push men to bury what they’re feeling sometimes behind long hours at work, intense workouts, or substance use. Physical symptoms like constant tiredness, poor sleep, or stomach issues are easier to talk about, but they can mask deeper emotional pain. And without safe, trusted spaces to open up, many Black men end up withdrawing or leaning on unhealthy coping strategies. Spotting these signs early and creating supportive, culturally aware spaces is key to helping Black men get the care they deserve.
What can you do to support Black men’s mental health?
Start the conversation
Ask: You’ve had a lot on your plate lately, how are you really feeling? or “I’ve noticed you’re not playing football lately, is everything okay?”
Tip: Choose a quiet moment and avoid distractions because it helps the person feel safe to open up.
Why it matters: Many Black men won’t volunteer how they’re feeling unless invited. A calm, open question can be the first step toward healing.
Challenge stigma
Say: “Struggling doesn’t make you weak, it makes you human.”
Tip: Share stories or articles that normalize emotional honesty, especially from relatable voices.
Why it matters: Cultural and gender norms often silence Black men, therefore challenging stigma helps dismantle barriers to seeking help.
Notice changes
Look for: A usually sociable friend becoming withdrawn, or someone suddenly irritable or reckless.
Tip: Keep a mental note of patterns such as small shifts over time can signal deeper issues.
Why it matters: Mental health struggles don’t always look like sadness, therefore spotting subtle changes can prevent prolonged suffering in silence.
Offer safe spaces
Create: A regular check-in group or WhatsApp wellness weekly chat where people can talk freely.
Tip: Make it informal, sometimes a walk, game night, or shared meal opens the door to real talk.
Why it matters: Safe spaces reduce fear of judgment and make it easier to open up before things escalate.
Share resources
Recommend: gone of the organisatons or advocacy groups below.
Tip: Frame it as “This might be helpful” rather than “You need this” — it reduces defensiveness.
Why it matters: Culturally competent care builds trust and ensures support is relevant and respectful.
Respect boundaries
Say: “I’m here when you’re ready – no pressure.”
Tip: Don’t take silence personally. Support is about presence, not pushing.
Why it matters: Pushing too hard can reinforce distrust. Respecting boundaries shows care without control.
Model openness
Share: “I’ve been feeling overwhelmed lately too, talking helped more than I expected.”
Tip: Vulnerability is contagious and your honesty can give others permission to speak up.
Why it matters: many Black men have never seen emotional openness modelled. Your example can shift what feels possible.
Educate yourself
Tip: Listen to podcasts, attend webinars, or follow Black mental health advocates on social media to stay informed.
Why it matters: understanding the intersection of race, masculinity, and mental health helps you show up with empathy and insight.
The information provided in this blog is for educational and informational purposes only and is not intended as medical advice. If you have questions about your health, speak to your GP or specialist.
If you need help or support, please consider reaching out to the following:
Samaritans
Website: samaritans.org
Phone: 116 123 (Free, 24/7 helpline)
Offers confidential emotional support for anyone in distress, including Black men navigating crisis or isolation.
Black Minds Matter UK
Website: blackmindsmatteruk.com
Phone: 0333 050 8671
Offers free therapy sessions with Black therapists to support mental health in Black communities.
Mandem Meetup
Website: mandemmeetup.org
Phone: 0775 158 9289
A grassroots peer support group creating safe spaces for Black men to connect and talk.
Mind
Website: mind.org.uk
Phone: 0300 123 3393 (Infoline) / 0300 102 1234 (Support Line)
National mental health charity with targeted programmes for young Black men and community outreach.
Reset MH
Website: resetmh.co.uk
Email: info@resetmh.co.uk
Focuses on mental health education and culturally relevant support for Black men and youth
The Empowerment Group
Website: theempowermentgroup.co.uk
Phone: 0790 833 6155
Provides mentoring, coaching, and emotional wellbeing support for Black men and boys.
Black Mental Health & Wellbeing Alliance (BMHWA)
Website: www.bmhwa.co.uk
A coalition advocating for structural reform in mental health services. Their Black Mental Health Manifesto calls for anti-racist, community-led approaches to care.
BAATN (Black, African and Asian Therapy Network)
Website: baatn.org.uk
Email: administrator@baatn.org.uk
A professional network offering access to therapists of Black, African, Asian, and Caribbean heritage.
Black Thrive
Website: blackthrive.org
Email: hello@blackthrive.org.uk
Works to address the impact of systemic racism on Black mental health through research and community action.

Leave a comment